Could Bacteria on Your Eyes Be Making Dry Eye Worse?

Dry eye disease is often described as a problem with tear production or tear evaporation. You’ve probably heard about artificial tears, punctal plugs, or omega-3 supplements if you’ve been battling the gritty, burning sensation of dry eyes. But what if there’s another piece of the puzzle that most people — and even some professionals — haven’t been paying enough attention to?
It turns out that your eyes, just like your gut and skin, have their own ecosystem of bacteria. This is called the ocular microbiome. It may sound strange at first — bacteria on your eyeballs? But far from being harmful, many of these microbes are actually essential to maintaining eye health. They help regulate inflammation, support the tear film, and keep potentially harmful pathogens in check.
However, when this microbial balance is disturbed — whether by environment, antibiotics, or even harsh eye drops — it can lead to or worsen dry eye symptoms. If your eyes feel perpetually irritated despite trying every lubricant under the sun, an imbalanced microbiome might be the hidden cause.
What Is the Ocular Microbiome?
The ocular microbiome refers to the collection of microorganisms — mostly bacteria, but also fungi and viruses — that live on the surface of the eye, especially the conjunctiva and eyelid margins. It’s a relatively low-biomass environment compared to places like your gut or mouth, but that doesn’t make it any less important.
The types of bacteria found here are generally non-pathogenic. Common species include Staphylococcus epidermidis, Corynebacterium, and Propionibacterium. In healthy eyes, these microbes live in harmony with each other and with your immune system. They’re part of the eye’s natural defence network, helping to outcompete potential invaders and reduce inflammation.
Recent studies have shown that these microbes communicate with immune cells and even with the cells that produce your tear film. That means your eye’s ability to stay moist and comfortable could be directly influenced by which bacteria are present — and in what balance.
How an Imbalanced Microbiome Can Trigger Dry Eye
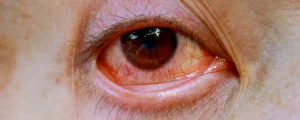
When the natural balance of bacteria on the eye is disrupted — a state called dysbiosis — your eye’s defences can become compromised. Harmful bacteria may gain the upper hand, inflammation levels can rise, and tear film stability may plummet.
Dysbiosis can happen for several reasons. One common culprit is the overuse of preservatives in eye drops. While meant to prevent contamination, preservatives like benzalkonium chloride (BAK) can harm beneficial bacteria and damage the delicate cells lining your eye. Long-term use may slowly change the makeup of your ocular microbiome.
Other factors include extended contact lens wear, use of antibiotics (oral or topical), and certain systemic diseases like diabetes or autoimmune conditions. Even excessive eye rubbing or poor lid hygiene can shift the microbial landscape.
The result? Increased inflammation, clogged Meibomian glands, and a disrupted tear film — all of which fuel the symptoms of dry eye.
The Link Between the Microbiome and Meibomian Gland Dysfunction
If you’ve been diagnosed with Meibomian Gland Dysfunction (MGD), the chances are high that your eye microbiome is also out of balance. MGD occurs when the oil-producing glands along your eyelid margins become blocked or inflamed. These oils are essential for preventing your tears from evaporating too quickly.
Certain bacteria produce lipases — enzymes that break down lipids. When these bacteria become overrepresented, their lipase activity can change the consistency of your natural oils, making them more waxy or sticky. This makes it harder for oil to flow freely, which in turn destabilises the tear film.
In some cases, bacterial biofilms — dense communities of microbes — can build up along the lash line, especially in chronic blepharitis. These biofilms are notoriously difficult to disrupt and act as breeding grounds for inflammation and further gland blockage.
How the Microbiome Affects Inflammation and Tear Stability
One of the most important functions of a healthy ocular microbiome is to keep inflammation in check. When the right bacteria are present, they communicate with the eye’s immune system to maintain a low level of immune activation. This helps preserve comfort and visual clarity.
But in dysbiosis, this calm balance is lost. The immune system starts reacting more aggressively, triggering chronic low-grade inflammation. This inflamed state damages the surface cells of the eye and makes them less capable of holding onto moisture. It can also affect the goblet cells, which produce the mucin layer of your tear film. Without mucin, tears can’t adhere properly to the eye, resulting in quicker evaporation.
This creates a vicious cycle: inflammation destabilises the tear film, and an unstable tear film worsens the environment for good bacteria — which leads to more inflammation.
Could Probiotics Help Treat Dry Eye?

Given how central the microbiome is to eye health, it’s no surprise that researchers are starting to explore probiotics as a potential therapy. Just like with gut health, the idea is to replenish beneficial bacteria to restore balance and reduce symptoms.
So far, most of the research on probiotics and dry eye has involved oral supplements. Some studies have shown that certain strains — like Lactobacillus casei or Bifidobacterium lactis — can reduce systemic inflammation and improve tear production indirectly by modulating the gut-eye axis.
Topical probiotics specifically designed for the eye are still in the early stages. However, the future looks promising. Experimental treatments using bacteriotherapy (reintroducing friendly strains directly to the ocular surface) have shown reductions in inflammation in early trials.
For now, maintaining a healthy gut through a diverse, fibre-rich diet may be one of the simplest ways to indirectly support your eye microbiome.
The Role of Eyelid Hygiene and Microbiome Preservation
If you want to preserve or restore your ocular microbiome, daily eyelid hygiene is a crucial step — but you have to get it right. Using overly harsh cleansers, antibacterial wipes, or chemical preservatives can do more harm than good. These products may kill off both good and bad bacteria indiscriminately.
Instead, opt for preservative-free, microbiome-friendly lid cleansers. Hypochlorous acid sprays, for instance, are gentle on tissues and help disrupt harmful biofilms without wiping out the whole ecosystem. Warm compresses followed by gentle lid massage can also help clear clogged glands and support natural oil flow.
If you wear makeup, always remove it thoroughly — especially around the lash line. Micellar cleansers are a good choice here, but avoid anything fragranced or alcohol-based. Ultimately, your aim should be to clean the area without sterilising it.
Antibiotics and the Microbiome: Use with Caution
Antibiotics, especially when used topically in the eye, can have a strong impact on the microbiome. While they’re sometimes necessary to control infection or inflammation, prolonged or repeated use can lead to a reduction in microbial diversity.
This is particularly relevant for people with recurrent blepharitis or MGD who have been placed on long-term courses of topical azithromycin or oral doxycycline. These medications may help symptoms initially, but they could be contributing to microbial imbalance if used indiscriminately.
If you’re on these medications and your dry eye symptoms are recurring or worsening, it may be time to discuss microbiome-supportive strategies with your specialist.
Can Contact Lenses Alter Your Eye’s Microbiome?

If you wear contact lenses — especially daily wear or extended wear lenses — it’s worth considering the impact they may have on your ocular microbiome. Although lenses themselves are sterile when first applied, their presence changes the environment of the eye in subtle but significant ways.
Studies have shown that contact lens wearers often have a microbial profile on their eyes that more closely resembles skin bacteria than the typical ocular flora. This shift likely occurs due to handling the lenses with fingers and placing them directly on the eye, which can transfer bacteria and disrupt the natural ecosystem. What’s more, lenses reduce oxygen exposure to the surface of the eye and can slightly raise surface temperature, creating conditions where some microbes thrive and others diminish.
This microbial shift isn’t just a curiosity — it may play a role in increasing inflammation, tear film instability, and Meibomian Gland Dysfunction. If you’ve developed dry eye symptoms while using contacts, switching to glasses for a few weeks (or using daily disposables with careful hygiene) might give your microbiome a chance to reset. And as research advances, contact lens solutions and materials designed to support microbiome health may become part of personalised dry eye management.
New Frontiers: Microbiome Testing and Personalised Dry Eye Care
One of the most exciting developments in the field is the emergence of ocular microbiome testing. Similar to stool tests for gut bacteria, these swab-based tests can analyse which microbes are present on your ocular surface and in what proportions.
While not yet in widespread clinical use, these tests may one day help guide more personalised treatments — identifying whether your symptoms are being driven by bacterial imbalance, inflammation, or gland dysfunction.
Imagine being able to treat dry eye based on your unique microbial signature, rather than a trial-and-error approach. That’s where things are heading — and it could be a game-changer for many patients who have been suffering without answers.
FAQ: Understanding the Microbiome and Dry Eye
- What exactly is the ocular microbiome?
The ocular microbiome refers to the community of bacteria and other microbes that naturally live on the surface of your eyes and eyelids. These organisms help regulate inflammation, support tear film health, and prevent infections — making them essential for eye comfort and protection. - How can bacteria cause or worsen dry eye symptoms?
When the normal balance of bacteria is disrupted — a state known as dysbiosis — it can lead to increased inflammation, tear film instability, and blocked glands. This disruption makes the eye more prone to dryness, irritation, and even secondary infections. - What causes microbiome imbalance in the eyes?
Common triggers include overuse of antibiotic or preservative-heavy eye drops, poor eyelid hygiene, long-term contact lens wear, or underlying conditions like rosacea or diabetes. Even something as simple as rubbing your eyes too often can affect microbial balance. - Can you test for problems with your eye microbiome?
While still emerging, ocular microbiome testing does exist and involves taking a swab from the surface of the eye. These tests can help identify the presence or absence of beneficial or harmful bacteria and may guide future treatment decisions. - Do antibiotics harm the eye microbiome?
Yes — especially when used long term. While antibiotics are helpful for controlling infections or inflammation, they can also kill off beneficial bacteria, which may worsen dry eye symptoms in the long run. - Are there any probiotics for the eyes?
Topical probiotics are still in early stages of research, but some oral probiotics may have beneficial effects through the gut-eye axis. Supporting gut health with a diverse diet may indirectly benefit your ocular surface. - What are the best lid hygiene products for preserving the microbiome?
Use gentle, preservative-free cleansers or hypochlorous acid sprays. Avoid antibacterial wipes or harsh soaps, which can disrupt microbial balance. Warm compresses combined with lid massage also support healthy gland function. - How does Meibomian Gland Dysfunction relate to bacteria?
Some bacteria produce enzymes that break down natural oils, making them thicker and harder to secrete. This contributes to blocked glands and destabilises the tear film, which are key features of MGD. - Can diet affect the ocular microbiome?
Yes — a healthy gut microbiome influences systemic inflammation, which can affect eye health. Diets rich in fibre, fermented foods, and healthy fats may help reduce inflammation and support a more balanced microbiome overall. - Should I avoid all preservatives in eye drops?
It’s best to use preservative-free drops whenever possible, especially if you’re using them frequently. Preservatives can damage the ocular surface and disrupt the microbial ecosystem, exacerbating dryness and irritation over time.
Final Thoughts: Rethinking Dry Eye from the Inside Out
If you’ve been treating dry eye purely from the outside — with drops, compresses, and plugs — and still not finding relief, it might be time to consider what’s happening on a microscopic level. The ocular microbiome is a vital, often-overlooked piece of the dry eye puzzle.
Supporting this delicate ecosystem means choosing your treatments carefully, being gentle with eyelid hygiene, and thinking beyond quick fixes. As research advances, you may even be able to restore microbial balance directly — offering hope for more lasting relief.
And if you’re seeking expert help with dry eye, ask whether your clinic considers the microbiome in their treatment protocols. At Eye Clinic London, we’re always exploring emerging dry eye treatment that go beyond the basics — because sometimes, the answers are hiding in plain sight.
References
- Li, J., Wang, H., Dong, X., Yu, J., Ma, S. and Sun, Q., 2024. What is the impact of microbiota on dry eye: a literature review of the gut‑eye axis. BMC Ophthalmology, 24, Article no. 262. Available at: https://bmcophthalmol.biomedcentral.com/articles/10.1186/s12886-024-03526-2 [Accessed 27 Jul. 2025].
- Uldry, A.C., Zysset‑Burri, D.C., Schlegel, I., Lincke, J.B., Jaggi, D., Keller, I. and Zinkernagel, M.S., 2024. The human ocular surface microbiome and its associations with dry eye disease. International Journal of Molecular Sciences, 24(18), 14091. Available at: https://www.mdpi.com/1422-0067/24/18/14091 [Accessed 27 Jul. 2025].
- Willis, K.A., Postnikoff, C.K., Freeman, A., Nichols, K. and Lal, C.V., 2020. The closed eye harbours a unique microbiome in dry eye disease. Scientific Reports, 10, 12035. Available at: https://www.nature.com/articles/s41598-020-68952-w [Accessed 27 Jul. 2025].
- Garbutt, J.S., Farhood, Z., Korblein, D., Asbell, P.A. and Abshire, R., 2023. Ocular microbiome changes in dry eye disease and meibomian gland dysfunction. Experimental Eye Research, XXX (online), published ahead of print. Available at: https://www.sciencedirect.com/science/article/pii/S0014483523002361 [Accessed 27 Jul. 2025].
- Song, Y., Xiao, K., Chen, Z. and Long, Q., 2022. Analysis of conjunctival sac microbiome in dry eye patients with and without Sjögren’s syndrome. Frontiers in Medicine, (Microbiome section). Available at: https://www.frontiersin.org/articles/10.3389/fmed.2022.841112/full [Accessed 27 Jul. 2025].

