Eye Problems in Children With Autism Spectrum Disorder

Autism affects how children process sensory information, including visual input. Even subtle vision problems can feel overwhelming or confusing for a child who already experiences sensory sensitivity. When visual issues go unnoticed, they may affect communication, focus, and daily functioning.
In this article, we explain common eye problems seen in children with autism and why they are sometimes missed. We also explore challenges during eye examinations and when specialist paediatric assessment is beneficial. This understanding helps you seek the right support at the right time.
Why Eye Problems Are Often Missed in Autism

Eye problems in children with autism are often missed because your child might not describe what they’re seeing in the usual way. They may not tell you that things look blurry or uncomfortable instead, you might notice changes in their behaviour.
You may see your child quietly avoiding tasks that require a lot of visual effort, or getting distressed in certain environments without an obvious reason. It’s easy to assume these behaviours are just part of autism, but they could be a sign of a vision problem.
Routine vision screening often relies on your child being able to communicate and cooperate. When that’s difficult, eye issues can go unnoticed. Being aware of this risk helps you make sure your child gets the care they need.
Refractive Errors in Children With Autism
Refractive errors, like short-sightedness, long-sightedness, and astigmatism, are quite common in children with autism. These conditions affect how clearly your child sees objects at different distances, and if left uncorrected, they can make learning and play more difficult.
You might notice your child struggling with glasses at first, especially if they have sensory sensitivities. The feel of frames on their face can be uncomfortable, but introducing glasses gradually and choosing the right frames can help them adjust more easily.
Once refractive errors are corrected, you’ll often see a noticeable improvement in engagement. Clearer vision can reduce frustration and help your child pay attention more easily. Even small changes can make a meaningful difference in their day-to-day life.
Strabismus and Eye Alignment Issues

Strabismus, which means misalignment of the eyes, occurs more often in children with autism. You may notice that one of your child’s eyes turns inwards, outwards, upwards, or downwards, either all the time or only in certain situations. This misalignment can affect depth perception and make seeing feel uncomfortable or confusing.
- Your child may not tell you something is wrong: Many children do not complain about double vision, even if their eyes are not working together properly. Instead, you might notice behaviours such as closing one eye, tilting the head, or avoiding activities that require close focus.
- Signs can be easy to miss: These behaviours are often subtle and may be mistaken for inattention or sensory avoidance. This is why careful observation and routine eye checks are so important.
- Early diagnosis protects binocular vision: Identifying strabismus early helps protect how the eyes work together. Without treatment, the brain may begin to ignore input from one eye, which can affect long-term vision development.
- Treatment options depend on your child’s needs: Treatment may include glasses, patching, or, in some cases, surgery. Starting treatment at the right time significantly improves visual outcomes and comfort.
Early assessment allows you to understand what your child needs and take action before vision problems become more difficult to treat. With timely intervention, many children achieve good eye alignment and improved visual function.
Amblyopia and Vision Development
Amblyopia, often called lazy eye, develops when one eye isn’t used properly during early childhood. This usually happens because of a squint (strabismus) or an uncorrected glasses prescription. If it’s not treated early, the reduced vision can become permanent.
When a child has autism, spotting amblyopia can be more difficult. You may find that standard eye tests don’t work well, especially if your child struggles with communication or unfamiliar environments. In these cases, eye specialists often rely on observation-based assessments instead.
You might notice signs such as favouring one eye, turning the head to look at objects, or avoiding close visual tasks. These subtle behaviours can provide important clues when formal testing isn’t possible. Parental observations are often a key part of the assessment.
The good news is that early treatment significantly improves outcomes. With adapted strategies, patience, and consistent support, many children respond well. Seeing a specialist who understands both vision development and autism can make a real difference to your child’s long-term sight.
Eye Movement and Focusing Difficulties
Some children with autism experience difficulties with eye movements and focusing. You may notice this when reading, tracking lines of text, or coordinating vision with hand movements feels harder than expected. As a result, everyday visual tasks can seem tiring or confusing.
When the eyes don’t work together effectively, visual discomfort can occur. You might see your child avoiding close work, losing concentration quickly, or appearing inattentive. These signs are easy to miss and are often mistaken for behavioural or attention-related issues.
A thorough eye assessment helps determine whether support or treatment is needed. With the right intervention, visual efficiency can improve. This often has a positive effect on learning, confidence, and daily activities.
Visual Processing Differences in Autism
Not all vision-related difficulties are caused by problems with the eyes themselves. Some children experience visual processing differences, where the brain finds it harder to interpret what the eyes see. This can affect how shapes, movement, depth, and space are perceived.
You may notice that busy visual environments feel overwhelming for your child. Patterned floors, crowded classrooms, or fast-moving images can increase anxiety or discomfort. As a result, your child may avoid certain spaces or become distressed.
Recognising visual processing differences helps prevent behaviour being misunderstood. A specialist assessment can clarify whether visual support strategies are needed. When you understand the underlying cause, it becomes much easier to put the right care and adjustments in place.
Sensory Sensitivities and Light Sensitivity
Light sensitivity is common in children with autism, and you may notice that bright lights, glare, or reflections cause your child discomfort or distress. This sensitivity can make everyday situations challenging and may also affect how your child responds during an eye examination.
- Your child may react to light in subtle ways: Instead of saying the light hurts, your child might squint, cover their eyes, turn away, or avoid certain rooms or outdoor spaces. These reactions are usually sensory responses rather than behavioural issues.
- Eye examinations can feel overwhelming: Examination lights and unfamiliar equipment can be difficult for a child who is sensitive to light. Understanding this helps clinicians adjust how assessments are carried out.
- Small adjustments make a big difference: Dimming lights, reducing glare, and allowing time for your child to settle can improve comfort and cooperation during assessments.
- A calm, flexible approach supports better outcomes: Creating a quieter, less stimulating environment reduces sensory overload. When your child feels more at ease, examinations are more accurate and less stressful for everyone involved.
Recognising light sensitivity helps you and your child’s clinician work together more effectively. With the right adjustments and a sensitive approach, eye assessments can be made more comfortable while still providing the information needed to support your child’s vision.
Challenges During Standard Eye Examinations
Standard eye examinations often rely on verbal instructions, eye contact, and sustained attention. For many children with autism, these expectations can be difficult, especially in an unfamiliar clinical setting. Anxiety can make it even harder for your child to engage or cooperate.
- Instructions may be hard to follow: Your child may struggle to understand or respond to spoken instructions, particularly if they are complex or delivered quickly. This can make it challenging for them to complete certain tests.
- Anxiety can affect cooperation: Bright lights, unfamiliar equipment, and new surroundings can increase anxiety. When your child feels overwhelmed, they may withdraw, become distressed, or refuse parts of the examination.
- Results may be incomplete or unclear: If your child is unable to fully engage, the results of a standard eye test may not accurately reflect their vision. This can leave you feeling uncertain or concerned that something has been missed.
- Specialist paediatric assessments take a different approach: Paediatric eye specialists adapt their testing methods to suit your child’s needs. They use flexibility, play-based techniques, and shorter testing sessions to improve comfort and accuracy.
When assessments are tailored to your child, examinations become less stressful and far more informative. A flexible, specialist approach leads to clearer results and a better experience for both you and your child.
How Specialist Paediatric Assessment Helps
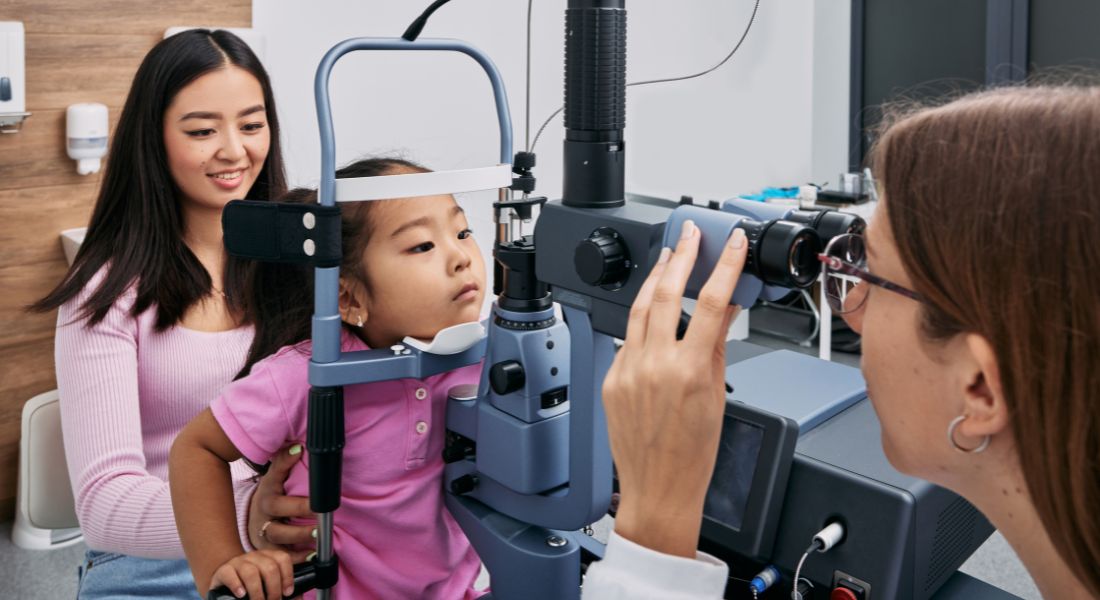
Specialist paediatric ophthalmologists use a child-centred approach to make eye assessments as comfortable as possible for your child. They adapt tests to your child’s developmental level and sensory needs, often using play-based or observation-based methods instead of standard procedures.
Examinations are paced to match your child’s tolerance, with breaks whenever they’re needed. Building trust comes first, and the focus is on understanding your child’s vision rather than rushing through the tests.
This approach not only helps achieve a more accurate diagnosis but also reduces stress for both your child and you. Seeing a specialist can really make a difference in managing vision concerns effectively.
Behavioural Signs That May Indicate Vision Problems
Vision difficulties in children can sometimes show up as changes in behaviour rather than obvious eye problems. You might notice your child avoiding visual tasks, becoming easily frustrated, or adopting unusual postures. Often, parents are the first to spot these patterns.
Some children hold objects very close to their eyes or tilt their head frequently when looking at things. Others may find busy visual environments overwhelming. These behaviours can be signs of visual discomfort.
Sharing what you observe with a specialist is really important. Your insight helps guide the assessment and ensures your child gets the right support. Working together with professionals can make a big difference in managing vision concerns.
The Link Between Vision and Behaviour Regulation
Your child’s vision can have a big impact on how they regulate their emotions and behaviour. When visual input is unclear, uncomfortable, or overwhelming, it can increase anxiety and make it harder for your child to stay calm and focused.
- Visual strain can affect behaviour: Some behaviours often attributed purely to autism such as avoiding eye contact, becoming frustrated during tasks, or withdrawing from activities may actually be influenced by visual discomfort or difficulty processing what they see.
- Understanding the connection changes how you can help: Recognising that vision plays a role in behaviour allows you and your child’s clinicians to address underlying causes rather than only managing the behaviour itself. This can lead to more effective support strategies.
- Meeting visual needs supports confidence: Correcting or managing visual issues through glasses, visual aids, or adapted environments can reduce strain and make tasks easier for your child. When vision is clear and comfortable, your child may engage more readily and feel more confident.
- Improved visual comfort benefits overall wellbeing: Supporting your child’s vision doesn’t just help them see better it can also reduce frustration, improve attention, and enhance emotional regulation. Clearer vision often leads to better participation in daily activities and a greater sense of wellbeing.
By understanding the link between vision and behaviour, you can provide support that addresses both your child’s visual and emotional needs, helping them navigate the world more comfortably and confidently.
When to Seek Ophthalmology Assessment
You should consider seeking an ophthalmology assessment if you notice signs of visual difficulty in your child. Changes in behaviour, struggles with learning, or avoidance of visual tasks can all be important clues trust your instincts.
Children with developmental conditions often benefit from proactive eye care. Even if there aren’t obvious symptoms, a baseline assessment can be very helpful. Early evaluation helps prevent problems from being missed.
A specialist review is especially valuable when routine eye checks don’t give clear answers. Tailored assessments can provide clarity and ensure your child receives the support they need. Timely referral plays a key role in protecting long-term vision development.
Supporting Children During Eye Appointments
You can make eye appointments much easier for your child with some simple preparation. Using visual schedules, giving clear and simple explanations, or sticking to familiar routines can help reduce uncertainty and lower anxiety.
Bringing comfort items and allowing breaks during the examination can make a real difference. Staying flexible is key progress matters far more than perfection.
Experienced clinicians know how to create a supportive and calm environment. With patience and understanding, they encourage cooperation, and positive experiences help build trust for future visits.
Treatment Adaptations for Children With Autism
Treatment plans for children with autism should be tailored to your child’s individual needs. Depending on their situation, this might include glasses, patching, or surgery, with adaptations to help your child accept and follow the plan.
It’s important to take sensory preferences into account. Lightweight frames, gradual wear schedules, or other small adjustments can make treatment much more comfortable. Working closely with you as a parent or caregiver helps improve outcomes.
Regular follow-up appointments ensure the treatment is working as it should. Plans can be adjusted when needed, and ongoing support is an essential part of comprehensive eye care.
Long-Term Vision Care and Monitoring
Your child’s vision needs can change as they grow, so regular monitoring is important to catch any new issues early. Consistent check-ups help support stable visual development over time.
Long-term care isn’t just about correcting vision it’s about comfort and function. Proper support can make learning easier and boost your child’s independence. Even small improvements can have a meaningful impact on daily life.
Working closely with clinicians is key. Open communication ensures your child’s needs are fully met, and continuity of care helps build confidence for both you and your child.
FAQs
- Are eye problems more common in children with autism?
Eye and vision problems are seen more often in children with autism than in the general population. This does not mean every autistic child will have an eye condition, but the likelihood is higher. Because autism affects sensory processing, even mild vision issues can have a bigger impact on how your child copes with daily activities. - How can you tell if your autistic child has a vision problem if they cannot explain it?
Many children with autism do not describe vision problems in words. Instead, you may notice changes in behaviour, such as avoiding reading, holding objects very close, tilting their head, or becoming distressed in visually busy environments. Trusting these observations is important, as they often provide the first clue that vision may be contributing to difficulties. - Can vision problems affect your child’s behaviour and learning?
Yes, unclear or uncomfortable vision can increase frustration, anxiety, and avoidance. When visual input feels overwhelming or confusing, your child may struggle to focus or regulate emotions. Addressing vision issues often improves engagement, confidence, and overall wellbeing. - Why do routine eye tests sometimes miss problems in autistic children?
Standard eye tests rely heavily on verbal responses and sustained attention, which may not suit your child’s communication style or sensory needs. If cooperation is limited, results may appear normal or incomplete. This can give false reassurance when a problem is actually present. - What types of eye problems are most common in children with autism?
Refractive errors, eye misalignment, amblyopia, and focusing or eye movement difficulties are all more frequently seen. Some children also experience light sensitivity or visual processing differences, where the eyes are healthy but the brain struggles to interpret what is seen. - Is light sensitivity a vision problem or a sensory issue?
Light sensitivity in autism is often sensory, but it can still cause significant visual discomfort. Bright lights, glare, or reflections may feel painful or overwhelming to your child. A specialist assessment helps determine whether there is an underlying eye condition or whether environmental adjustments are the main solution. - When should you seek a specialist paediatric ophthalmology assessment?
You should consider specialist assessment if routine eye checks are inconclusive, if your child resists testing, or if you notice ongoing behavioural or learning concerns that may be visually related. Even without obvious symptoms, proactive assessment is helpful for children with developmental conditions. - How are eye examinations adapted for children with autism?
Specialist paediatric ophthalmologists use flexible, child-centred approaches. Testing may involve play, observation, pictures, or movement rather than verbal answers. The pace is adjusted to your child’s tolerance, with breaks and reassurance to reduce anxiety. - Can autistic children adapt to wearing glasses or eye treatments?
Many children initially find glasses or patching difficult due to sensory sensitivity, but with the right support, most adapt well. Choosing comfortable frames, introducing wear gradually, and following your child’s cues makes a big difference. Improvement in vision often increases acceptance over time. - Will your child need ongoing eye care as they grow?
Yes, vision can change throughout childhood, and regular monitoring is important. Ongoing care ensures new problems are detected early and treatments remain effective. Long-term support focuses on comfort, function, and helping your child engage more confidently with the world around them.
Final Thought: Why Early Eye Assessment Matters in Autism
If you are caring for a child with autism and feel unsure whether vision may be contributing to behaviour, learning, or sensory challenges, it is always worth seeking clarity. Eye problems in autistic children are often subtle, easily missed, and can look very different from those seen in neurotypical children. When visual discomfort or reduced vision goes unrecognised, it can quietly add to daily stress for both you and your child.
A specialist assessment can make a meaningful difference by using child-centred, flexible approaches that respect sensory and communication needs. Seeing an experienced paediatric ophthalmologist in London who understands autism and developmental conditions allows concerns to be explored gently and thoroughly, even when standard eye tests have not been helpful. Early understanding supports better comfort, confidence, and long-term visual development. If you’d like to find out whether seeing a paediatric ophthalmologist in London is suitable for you and your child, feel free to contact us at Eye Clinic London to arrange a consultation.
References:
- Kayıtmazbatır, E.T., Güler, H.A., Duyan, Ş.A., Oflaz, A.B. and Bozkurt, B. (2025) ‘Visual health in autism spectrum disorder: screening outcomes, clinical associations and service gaps’, Medicina, 61(10), p.1779. https://www.mdpi.com/1648-9144/61/10/1779
- Demir, Ü., Kocamaz, M. and Özdemir, G. (2021) ‘Ocular findings and refractive errors in children with autism spectrum disorder’, Children, 8(6), p.606. https://www.mdpi.com/2227-9067/10/4/606
- Mazurek, M.O. and Wenstrup, C. (2013) ‘Ophthalmologic disorders in children with autism spectrum disorder’, https://pubmed.ncbi.nlm.nih.gov/23836398
- Evaluation of ocular findings in children with autism spectrum disorder: Observational study (2025) Wolters Kluwer Health, Inc. https://pubmed.ncbi.nlm.nih.gov/40696676/
- Demir, U. (2025) ‘Evaluation of ocular findings in children with autism spectrum disorder: Observational study’, Medicine (Baltimore). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC12282795

