Does Glaucoma Always Affect Both Eyes? (Guide)

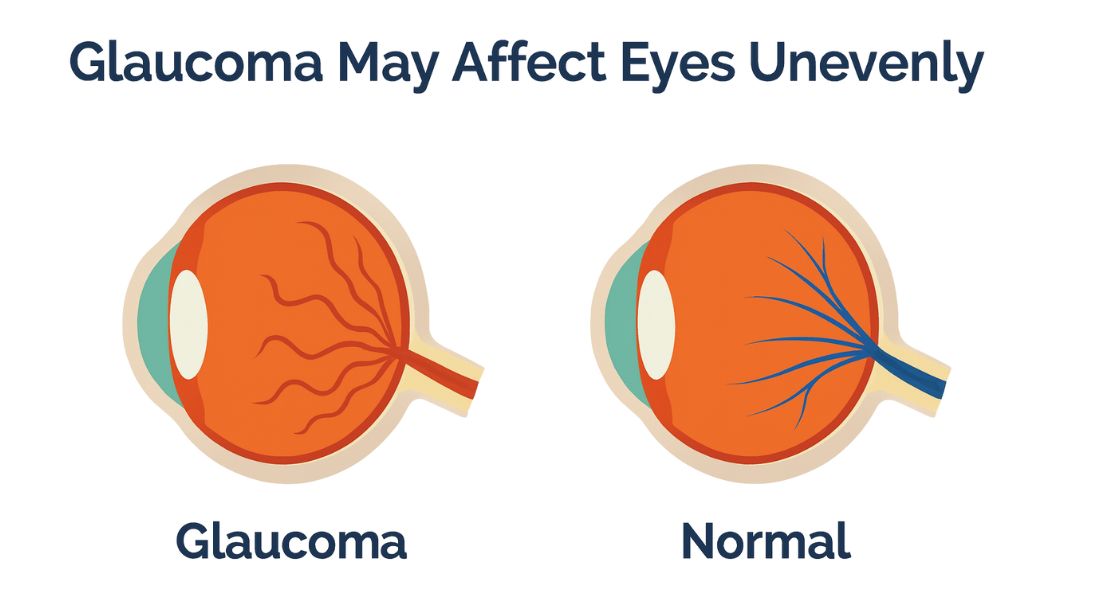
Many people are surprised to learn that glaucoma does not always affect both eyes in the same way. You might be told that one eye shows clear signs of damage while the other seems relatively normal. This uneven pattern can feel confusing and even worrying at first.
Glaucoma is a condition that affects the optic nerve, and each eye has its own nerve, blood supply, and structural characteristics. Because of these differences, glaucoma can begin in one eye or progress faster in one eye than the other. In fact, this asymmetry is very common, so it doesn’t necessarily mean something has been missed.
In this article, you will learn whether glaucoma always affects both eyes, why it can start or worsen unevenly, and how your treatment plan accounts for these differences. Understanding this can help you feel more confident about your diagnosis and the care decisions your eye specialist recommends.
Understanding Glaucoma as a Bilateral Disease
Glaucoma is generally considered a bilateral condition, which means it has the potential to affect both eyes. However, bilateral does not mean that both eyes are affected in the same way or at the same rate. Each eye can behave very differently over time.
The disease process may exist in both eyes even if detectable damage appears in only one. Early changes are often subtle and can be difficult to measure with standard tests. This can give the impression that only one eye is affected, even when the other is quietly at risk.
As time goes on, many people do develop glaucoma in both eyes. The main difference lies in timing and severity. Asymmetry is a key feature of glaucoma, and recognising this helps you understand why monitoring both eyes closely is essential.
Why One Eye Can Be Affected First
Glaucoma may begin in one eye because that eye is more vulnerable to damage. Small structural differences in the optic nerve can make one side less resilient than the other, and even minor variations can have a significant impact over time.
Blood flow to the optic nerve can also differ between eyes. If one eye receives slightly less perfusion, it becomes more susceptible to damage. This can lead to earlier changes in that eye, even before the other shows any signs.
These differences are usually invisible without testing. You won’t feel them, and routine activities won’t reveal the problem. This is why glaucoma often seems to “pick” one eye first, even though both are at risk.
Structural Differences Between the Eyes
No two eyes are perfectly identical. The shape of the optic nerve head and the thickness of nerve fibres vary naturally from one eye to the other. These differences can influence your risk of developing glaucoma and how it progresses.
For example, one eye may have a thinner nerve fibre layer, making it more vulnerable to pressure-related damage. Even normal eye pressure can cause harm if the nerve is less robust.
This structural asymmetry helps explain why glaucoma can progress at different rates in each eye. It’s a natural, biological variation not a sign that treatment has failed. Your care is personalised to account for these differences and protect both eyes as effectively as possible.
Intraocular Pressure Differences Between Eyes
Your eye pressure is rarely exactly the same in both eyes, and small differences are completely normal. Understanding these variations helps explain why glaucoma can progress differently in each eye. Paying attention to each eye individually ensures the best long-term protection for your vision.
- Small differences are normal: Most people have slight pressure variations between their eyes. These minor differences usually don’t cause problems but are monitored over time.
- Persistent asymmetry can increase risk: If one eye consistently has higher pressure, it may develop damage sooner than the other. Even a few millimetres of difference can be significant, depending on your individual sensitivity.
- Each eye may need personalised management: Because pressure sensitivity varies from person to person, treatment can be tailored for each eye separately. Regular monitoring ensures both eyes are protected appropriately.
Measuring both eyes individually is key to effective glaucoma care. It allows your specialist to catch early changes and intervene before significant damage occurs. Treatment plans are customised to your unique pressure profile. By monitoring each eye carefully, you give yourself the best chance of preserving long-term vision.
Normal-Tension Glaucoma and Asymmetry
Glaucoma can develop even when eye pressure remains within the normal range, a condition known as normal-tension glaucoma. In these cases, asymmetry between the eyes is common, with one eye often more affected than the other.
Here, eye pressure alone does not explain the damage. Factors such as blood flow, vascular health, and individual nerve susceptibility play a larger role in progression.
This type of glaucoma highlights why relying solely on pressure measurements is insufficient. Comprehensive assessment, including structural and functional tests, is essential. Each eye must be evaluated independently to ensure subtle changes are not missed.
Why Symptoms May Appear in Only One Eye
You might notice changes in one eye while the other seems fine, which can be worrying or confusing. Early glaucoma often progresses unevenly, so one eye may show more damage before the other. Understanding this helps you interpret what you see and why regular testing is essential.
- Peripheral vision may be affected unevenly: One eye can lose side vision faster than the other. Your brain often compensates by relying on the stronger eye, which masks early signs of the problem.
- The “healthy” eye can be misleading: Just because you don’t notice symptoms in one eye doesn’t mean it’s unaffected. Early changes may still be happening silently.
- Testing reveals the full picture: Regular eye examinations allow your specialist to detect changes in both eyes, even before you notice them. This ensures timely intervention and better protection for your vision.
Symptoms appearing in only one eye can give a false sense of security. Understanding how glaucoma progresses helps you take proactive steps. Testing both eyes thoroughly is the only way to know what’s really happening. By staying vigilant, you protect both eyes and your long-term sight.
Visual Field Loss and Eye-to-Eye Differences
Visual field testing often reveals differences between the eyes, with one eye showing clear defects while the other may appear normal. This asymmetry is common, especially in early glaucoma.
Because visual field loss develops gradually, early defects can be subtle and easily missed. Repeated testing over time improves detection and helps track progression accurately.
Monitoring each eye individually is crucial. Progression can vary between eyes, and treatment decisions rely on understanding these patterns. Careful, eye-specific assessment ensures optimal management.
Optic Nerve Appearance in Asymmetric Glaucoma
Your optic nerves may not look identical, and differences can be an early clue to glaucoma. One nerve may show thinning or “cupping” before the other, even if your vision feels normal. Recognising these differences helps your eye specialist make an accurate diagnosis and plan the right care.
- Small differences can be significant: Ophthalmologists carefully compare the optic nerves in both eyes. Even subtle changes can indicate early glaucoma and guide decisions about monitoring or treatment.
- Imaging enhances detection: Advanced scans and imaging provide detailed views of the optic nerve. This helps detect asymmetry that might not be obvious in a standard exam.
- Asymmetry prompts closer attention: Noticing differences between eyes acts as a red flag. It usually leads to more frequent monitoring and early intervention to protect your vision.
Differences in optic nerve appearance can reveal glaucoma before symptoms appear. Careful assessment allows your specialist to act early and prevent further damage. Even small changes matter when it comes to protecting your sight. Being aware of these signs ensures both eyes get the attention they need.
How Imaging Detects Subtle Asymmetry
Modern imaging tools can measure the thickness of optic nerve fibres with remarkable precision. These scans often reveal changes before any symptoms arise, making asymmetry between the eyes visible early.
Imaging compares each eye to established normative databases and also evaluates differences between your own eyes. This dual approach enhances diagnostic accuracy and helps detect early disease.
These tools explain why glaucoma is sometimes diagnosed in one eye before the other. Even if one eye appears healthy, it may still be at risk, so ongoing surveillance remains essential.
Why Glaucoma Rarely Progresses Equally
You might notice that glaucoma affects your eyes differently, even if you follow treatment exactly. Progression depends on several factors, including eye pressure, blood flow, nerve resilience, and individual anatomy all of which can vary between your eyes. Recognising this helps you understand why changes may appear uneven and reduces unnecessary worry.
- Multiple factors influence progression: Each eye responds differently to pressure and blood flow. The strength and resilience of the optic nerve also vary, affecting how quickly damage occurs.
- Treatment does not guarantee identical outcomes: Even with the same medication or therapy, one eye may remain stable while the other shows gradual change. This variability is a normal part of glaucoma.
- Management is tailored to each eye: Specialists monitor each eye individually and adjust treatment as needed. Personalised care ensures both eyes are protected as effectively as possible.
Uneven progression is an expected part of glaucoma. Understanding this helps you stay patient and focused on long-term management. Your treatment plan adapts to how each eye responds. By monitoring carefully, you give yourself the best chance of preserving vision in both eyes.
How Treatment Plans Address Eye-to-Eye Differences
Glaucoma treatment is often customised for each eye. One eye may need more aggressive pressure-lowering therapy, while the other may be managed with observation or milder intervention.
Medications can be adjusted differently between eyes, and procedures like laser or surgery may sometimes be necessary for just one eye. This individualised approach is common and reflects the asymmetrical nature of the disease.
The ultimate goal is to protect vision in both eyes. Tailoring treatment to each eye improves outcomes and ensures no eye is neglected. In glaucoma, one-size-fits-all strategies rarely work.
Medication Response Can Differ Between Eyes

When you use glaucoma eye drops, you may notice that one eye responds better than the other and that’s completely normal. Differences in tissue response mean pressure reduction can vary, even with the same treatment. Understanding this helps you see why your specialist may adjust therapy differently for each eye.
- Eye drops may affect each eye differently: One eye might achieve the target pressure while the other remains slightly higher. This variability is a common and expected part of glaucoma management.
- Treatment is tailored to each eye: If one eye isn’t responding adequately, your doctor may escalate therapy or try a different medication. Meanwhile, the other eye may remain stable on the original drops.
- Separate monitoring ensures safety: By checking each eye individually, your specialist can make timely adjustments. This personalised approach helps protect both eyes and reduce the risk of progression.
Response to medication can vary from one eye to the other. Monitoring each eye separately ensures that treatment meets your specific needs. Adjustments are made as required to keep pressure under control. Flexibility in management gives you the best chance of preserving vision in both eyes.
Laser Treatment and Asymmetry
Laser procedures for glaucoma are sometimes performed on one eye before the other. The decision depends on disease severity, progression rate, and risk to vision. Targeting the eye with more advanced changes allows early intervention where it is most needed.
Responses to laser treatment can vary between eyes. One eye may achieve excellent pressure control, while the other may respond more slowly or inadequately. Monitoring both eyes ensures any differences are detected promptly.
A staged approach helps balance benefits and risks. Treating both eyes simultaneously is not always necessary and may increase potential complications. Careful planning maximises safety and effectiveness.
Asymmetry guides clinical decision-making throughout the process. Each eye is treated based on its individual status, progression, and response, ensuring tailored, optimal care.
Surgical Decisions in Uneven Glaucoma
When glaucoma affects your eyes differently, surgery is usually planned carefully rather than treating both eyes at once. Your specialist often operates on one eye first, using the outcome to guide decisions for the other eye. This approach balances effectiveness with safety, ensuring each eye receives the care it needs.
- Priority is based on severity: If one eye shows more advanced damage, it may be treated sooner. The other eye can often be managed conservatively until surgery is truly necessary.
- Staged surgery reduces risk: Performing procedures separately allows your specialist to monitor recovery and adjust the plan for the second eye. This careful approach minimises complications and protects overall vision.
- Each eye is considered independently: Decisions are based on the specific condition and needs of each eye, rather than applying a one-size-fits-all plan.
Staged surgery ensures that each eye receives appropriate attention. It allows your specialist to learn from the first procedure and optimise care for the second. Safety and effectiveness are prioritised at every step. Treating eyes independently helps protect your long-term vision.
Monitoring Frequency for Each Eye

Follow-up schedules can vary significantly between your eyes. The eye that shows more signs of glaucoma is usually monitored more closely, while the other eye may have longer intervals between appointments. Testing frequency is carefully tailored to the level of risk in each eye, ensuring that any changes or progression are detected as early as possible. This approach allows your clinician to respond quickly if one eye starts to worsen.
Visual field assessments and imaging tests, such as optical coherence tomography (OCT), may be repeated more often for the affected eye. These tests help track subtle changes in nerve fibre thickness and function over time. Meanwhile, the other eye is still examined regularly, even if it appears stable, to make sure that early signs of glaucoma are not missed. This dual approach balances vigilance with practicality.
Psychological Impact of One-Eye Diagnosis
Being told that only one eye is affected by glaucoma can feel unsettling. You may worry that the other eye will suddenly develop the condition. These feelings of anxiety and uncertainty are very common, and it’s natural to feel concerned about your long-term vision.
Understanding that asymmetry is normal can help ease these fears. Glaucoma progression is usually slow, and regular monitoring is in place to protect the fellow eye. Knowing that your eye care team is keeping a close watch can provide reassurance and a sense of control over the situation.
Education and support play a crucial role in coping with a one-eye diagnosis. The more you understand about how glaucoma behaves, the better you can manage your expectations and take proactive steps. Feeling informed empowers you, reduces anxiety, and helps you stay confident in your care plan.
When the Second Eye Becomes Involved
In many cases, the second eye develops glaucoma changes over time, and this can take several years. Early detection is key because it allows any damage to be limited before it affects your vision significantly. Regular monitoring helps ensure that you are aware of changes as soon as they begin.
Because the second eye is carefully observed, any signs of progression are caught early. Your treatment plan can then be adjusted promptly, whether that means changing medication or considering other interventions. This proactive management helps protect your vision and maintain eye health over the long term.
This vigilant approach explains why outcomes for glaucoma are often positive. Continuous surveillance and timely treatment make a real difference. Prevention isn’t a one-off it’s an ongoing process that helps you retain as much vision as possible in both eyes.
Common Myths About One-Eye Glaucoma
Some people believe that glaucoma can only affect one eye. In reality, this is rarely true over the long term. While one eye may show damage first, the disease has the potential to affect both eyes eventually.
Others assume that the unaffected eye will remain healthy forever. This is a risky assumption, as glaucoma can develop slowly and silently. Regular check-ups are essential to catch any early changes and adjust treatment if needed.
Dispelling these myths is important for protecting your vision. Understanding the true nature of glaucoma encourages you to follow monitoring schedules and treatment plans. Education acts as a form of preventive care, helping you maintain sight in both eyes.
Who Is More Likely to Have Asymmetric Glaucoma
Glaucoma does not always affect both eyes equally. In many cases, one eye may show more damage or progress faster than the other. Certain risk factors make asymmetric glaucoma more likely, helping doctors identify who needs closer, eye-specific monitoring.
| Risk Factor | Why Asymmetry Is More Likely |
| Normal-tension glaucoma | Vascular differences |
| High myopia | Structural vulnerability |
| Unequal eye pressure | Pressure sensitivity |
| Vascular disease | Blood flow imbalance |
| Older age | Reduced nerve resilience |
Summary: Why Glaucoma Can Affect Eyes Differently
Glaucoma does not always affect both eyes equally. Differences in optic nerve structure, eye pressure, blood flow, and individual healing responses can cause one eye to be more vulnerable than the other. Understanding these factors helps explain why asymmetry is common and why each eye requires careful, personalised monitoring.
| Factor | Effect on Asymmetry |
| Optic nerve structure | Unequal susceptibility |
| Eye pressure | Different damage rates |
| Blood flow | Variable nerve health |
| Healing response | Uneven progression |
| Treatment response | Eye-specific outcomes |
FAQs:
- Does glaucoma always affect both eyes at the same time?
Glaucoma does not necessarily affect both eyes simultaneously. It can start in one eye and progress more slowly or differently in the other. Each eye has unique structural and vascular characteristics that influence when and how the disease develops. - Can one eye be worse than the other?
Yes, it is common for one eye to show more advanced damage than the other. Differences in optic nerve strength, nerve fibre thickness, or blood flow can cause one eye to deteriorate sooner. This asymmetry is normal and does not indicate treatment failure. - Is it possible to have glaucoma in one eye only?
While glaucoma can appear to affect only one eye initially, the other eye often remains at risk. Subtle changes may already be occurring in the second eye, which is why regular monitoring is essential. - Why does eye pressure differ between my eyes?
Eye pressure is rarely identical in both eyes. Small differences are natural, but persistent asymmetry can influence the risk of glaucoma. One eye may be more sensitive to pressure or more prone to damage, affecting how quickly glaucoma develops. - How do doctors detect glaucoma if it seems one-sided?
Doctors use a combination of visual field testing, optic nerve examination, and advanced imaging to assess each eye independently. These tools can detect subtle asymmetry, helping to identify early changes even when one eye appears healthy. - Can glaucoma progress unevenly even with the same treatment?
Yes, treatment response can vary between eyes. One eye may achieve stable pressure while the other continues to show changes, which is why management is often tailored for each eye separately. - When is surgery considered for asymmetric glaucoma?
Surgery is usually considered for the more affected eye first. This staged approach allows the outcome to guide future treatment for the other eye. It helps balance risks and ensures close monitoring for any changes. - Does having glaucoma in one eye increase the risk for the other?
Having glaucoma in one eye does increase the risk for the fellow eye. However, regular monitoring and early intervention can often prevent or slow damage, preserving vision in both eyes. - Why do some patients develop normal-tension glaucoma in only one eye first?
Normal-tension glaucoma can appear asymmetrically because pressure is not the only factor. Blood flow differences, optic nerve vulnerability, and individual anatomical factors can cause one eye to show damage earlier than the other. - How often should each eye be monitored if glaucoma appears asymmetric?
Monitoring frequency depends on each eye’s condition. The more affected eye may require more frequent visual field tests and imaging, while the other eye is still regularly checked. Personalised schedules ensure progression is caught early and treatment can be adjusted promptly.
Final Thought: Asymmetric Glaucoma and Monitoring
Glaucoma does not always affect both eyes in the same way, and asymmetry is more common than many patients realise. Understanding that one eye may be more vulnerable or progress differently helps reduce anxiety and highlights the importance of regular, personalised monitoring. Early detection and tailored treatment are key to preserving vision over time.
If you’re concerned about how glaucoma may be affecting your eyes, or want guidance on managing uneven progression, it’s important to seek professional advice. If you’d like to find out whether glaucoma treatment in London is suitable for you, feel free to contact us at Eye Clinic London to arrange a consultation.
References:
- Leske, M.C., Heijl, A., Hussein, M., et al. (2020) Interocular asymmetry of visual field loss and intraocular pressure in primary open‑angle glaucoma, Karger Ophthalmologica, 234(4), pp.219–227. https://pubmed.ncbi.nlm.nih.gov/32759608/
- Tan, A. and Wong, T. (2011) Extent of asymmetry and unilaterality among juvenile onset primary open‑angle glaucoma patients, Clinical and Experimental Ophthalmology, 39(9), pp.843–849. https://pubmed.ncbi.nlm.nih.gov/21631667/
- Hou, H., Moghimi, S., Zangwill, L.M., et al. (2018) Inter‑eye asymmetry of optical coherence tomography angiography vessel density in bilateral glaucoma, glaucoma suspect, and healthy eyes, American Journal of Ophthalmology, 190, pp.1–10. https://www.sciencedirect.com/science/article/abs/pii/S0002939418301272
- Medeiros, F.A. and Weinreb, R.N. (1989) Unequal intraocular pressure and its relation to asymmetric visual field defects in low‑tension glaucoma, Ophthalmology, 96(9), pp.1312–1314. https://www.sciencedirect.com/science/article/abs/pii/S0161642089327217
- Rodríguez‑Robles, F., Verdú‑Monedero, R., Berenguer‑Vidal, R., et al. (2023) Analysis of the asymmetry between both eyes in early diagnosis of glaucoma combining features extracted from retinal images and OCTs, Sensors, 23(10), p.4737. https://www.mdpi.com/1424-8220/23/10/4737

