Is PRK Surgery Safe for Dry Eyes?
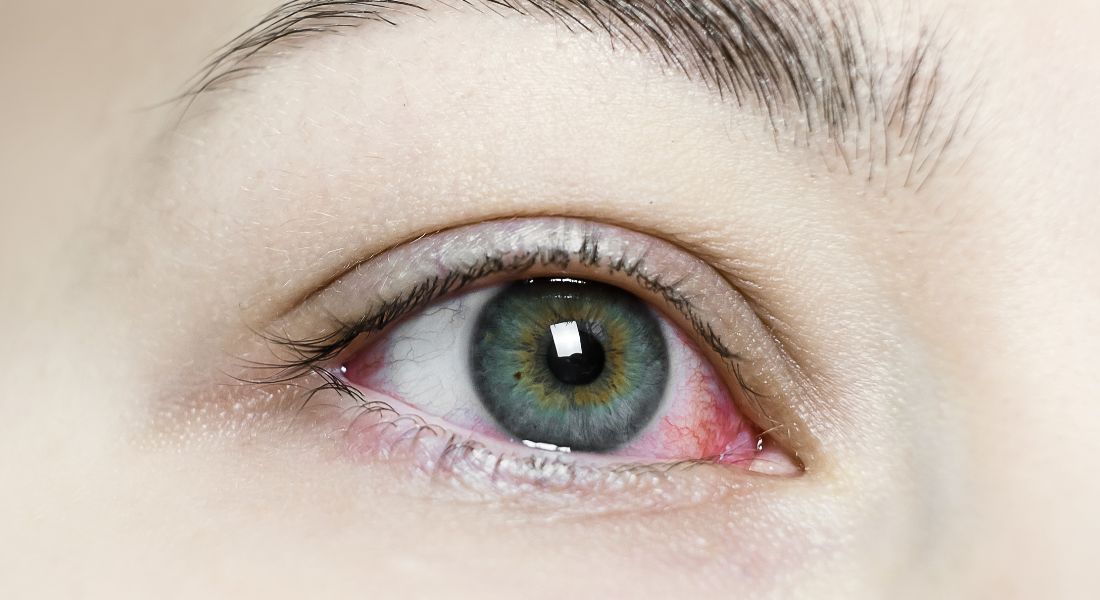
If you’re living with dry eyes and thinking about laser vision correction, you’ve probably come across a lot of conflicting advice. Maybe you’ve heard that LASIK can worsen dry eye symptoms or that you’re automatically unsuitable for laser treatment altogether. Many people assume dry eyes rule them out completely but that isn’t true. In many cases, PRK (Photorefractive Keratectomy) is actually one of the safest and most appropriate options for people with dryness.
I’ve spoken with countless patients who were told that LASIK wasn’t suitable because their tear film was unstable or their corneas were too dry, only to later discover that PRK could still give them clear, comfortable vision without worsening their symptoms long-term. It’s a procedure that avoids creating a corneal flap and can therefore be better tolerated by dry-eye–prone eyes, especially as we get older or spend long periods on digital devices.
In this guide, I want to walk you through exactly why PRK is considered safer for dry eyes, how it affects the tear film, what you can expect during recovery, and how to decide whether it’s the right procedure for you.
Why Dry Eyes Matter in Laser Vision Correction
Dry eyes aren’t just a minor inconvenience — they play a major role in how your vision stabilises after surgery. Your tear film is the first refractive surface of your eye, meaning it influences how crisp and clear your vision appears. If the tear layer is unstable, your eyesight can fluctuate or feel blurry, making post-surgery recovery less predictable.
Dry eyes can cause:
Burning or stinging: This happens when the tear layer evaporates too quickly, leaving the surface exposed and irritated.
Grittiness: Many people describe it as a sandy or dusty sensation, especially toward the end of the day.
Blurred vision: An uneven tear film scatters light, making your sight appear smeared or foggy.
Eye fatigue: Your eyes work harder to maintain focus, which can lead to tiredness and strain.
Fluctuating clarity: Vision may be sharp at one moment and hazy the next, depending on tear film stability.
Light sensitivity: Dryness can make bright lights feel harsher, particularly in windy or air-conditioned environments.
Difficulty wearing contact lenses: Lenses rely on a healthy tear film to stay comfortable, so dryness can make them feel intolerable.
When laser surgery enters the picture, a dry eye assessment becomes even more important. Proper evaluation ensures your eyes are stable enough for treatment and helps tailor the procedure to give you the best long-term visual outcome.
Why LASIK Can Make Dry Eyes Worse
Many people with dry eyes are advised against LASIK, and here’s why. Even mild pre-existing dryness can become more problematic after the procedure, affecting comfort and visual clarity.
During LASIK, a flap is created in the cornea. This process disrupts the corneal nerves that help regulate tear production. When these nerves are cut, the eye may not realise it’s dry, so it produces fewer tears. The temporary loss of nerve function can take several months to fully recover, prolonging dryness symptoms.
Effects of LASIK on dry eyes:
Nerve disruption – Corneal nerves are partially severed during flap creation, which slows the eye’s ability to sense dryness.
Reduced tear reflex – With diminished nerve input, tear production decreases, making lubrication less effective.
Temporary inflammation – Surgical trauma can trigger mild inflammation, which can worsen discomfort and delay healing.
More fluctuating vision in dry-eye–prone patients – Without a stable tear film, vision may blur intermittently, especially during reading or screen use.
Higher risk of symptoms during the early months – Patients may experience burning, grittiness, or light sensitivity as the nerves gradually recover.
For people with pre-existing dryness, this can make symptoms noticeably worse, even if the surgery itself is technically safe. This is where PRK becomes a better alternative, as it avoids creating a flap and preserves more corneal nerves, reducing the risk of worsening dry eye.
Why PRK Is Often Safer for Dry Eyes

PRK is a surface-based procedure, which means that unlike LASIK, no corneal flap is created. Instead, the surgeon removes only the outermost layer of the cornea, called the epithelium, which then regenerates naturally over time. This approach preserves the deeper corneal structures and nerves, which are important for maintaining healthy tear production.
For patients with dry eyes, PRK offers several advantages. Because no flap is made, fewer corneal nerves are disrupted, allowing the tear film to stabilise more quickly after surgery. This reduces the risk of long-term dryness and discomfort. Additionally, the cornea remains structurally stronger since its deeper layers are left intact.
Patients who already have borderline tear function often find PRK more comfortable than LASIK. While the procedure still temporarily affects the tear film, the overall impact on eye moisture and comfort is generally milder, making it a safer option for those prone to dry-eye symptoms.
Overall, PRK’s surface-focused technique provides a gentler approach for maintaining corneal health and tear stability, which is particularly beneficial for individuals concerned about dry eyes.
How PRK Works
Understanding the procedure can help you see why it’s often recommended for people with dry eyes. By working on the surface rather than creating a flap, PRK minimises disruption to the nerves that control tear production.
Steps of PRK:
The epithelium is gently removed.
This thin outer layer is cleared to expose the cornea for precise laser treatment. The process is quick and does not affect the deeper structural tissue.
A laser reshapes the cornea to correct the prescription.
The surface is sculpted to adjust focusing power. Because the deeper corneal layers remain untouched, the eye retains more of its natural strength.
A bandage contact lens is placed on the eye while the epithelium heals.
This protective lens reduces discomfort and shields the surface as new cells regenerate. Most patients wear it for 3–5 days.
The surface regenerates over 3–5 days.
The epithelium grows back naturally, forming a smooth, healthy layer. During this time, vision may be slightly hazy but gradually improves.
Vision gradually improves over the following weeks.
As healing continues, visual clarity stabilises, and most patients notice steady improvement week by week.
Because the corneal nerves responsible for tear reflex sit deeper than the surface, PRK interferes with fewer nerves compared with LASIK.
What Dryness Feels Like After PRK

Experiencing dryness after PRK is a normal part of the healing process, though it often feels different from dryness after LASIK. Many patients notice mild dryness during the first few weeks, sometimes accompanied by occasional burning, fluctuating vision, or light sensitivity. Blinking may also feel slightly uncomfortable as the corneal surface regenerates.
The timeline for dryness varies, but most people see steady improvement as the eye heals. During the first week, mild to moderate dryness is common while the epithelium repairs itself. Between weeks two and six, the tear film gradually stabilises, helping reduce discomfort. By three to six months, most patients experience a significant reduction in dryness.
Those with pre-existing dry eyes often tolerate PRK better than LASIK. Because PRK avoids creating a corneal flap, it disrupts fewer nerves, allowing the eye to heal more naturally. This results in a gentler recovery and generally less long-term dryness, making PRK a preferred option for patients prone to dry-eye symptoms.
Why PRK Doesn’t Cause Long-Term Dry Eyes the Same Way LASIK Can
The difference in long-term dryness between PRK and LASIK comes down to how each procedure affects the corneal nerves. Corneal nerves play a crucial role in maintaining a healthy tear film, and the more nerves that are disrupted, the greater the risk of prolonged dryness.
During LASIK, a corneal flap is created, which cuts through deeper nerves and can significantly impact tear production. In contrast, PRK only affects the surface nerves temporarily, leaving the deeper nerve network intact. This allows the cornea to maintain better long-term function and reduces the likelihood of chronic dryness.
Because of this nerve-sparing approach, PRK is often recommended for patients with pre-existing dry-eye issues, contact lens intolerance, autoimmune-related dryness, or mild tear-film dysfunction. By avoiding deep nerve disruption, PRK offers a safer option for preserving long-term ocular comfort and tear stability.
Who Makes a Good Candidate for PRK if You Have Dry Eyes?

PRK can be a suitable option for people with mild to moderate dry-eye symptoms. It’s particularly considered when corneal thickness is borderline for LASIK, or when the tear breakup time (TBUT) is low, indicating that the tear film is less stable.
People who experience discomfort with contact lenses, or who work in dusty, dry, or high-impact environments, may also benefit from PRK. Because the procedure avoids creating a flap, it preserves corneal nerves and supports healthier tear film function over the long term.
Ultimately, candidacy for PRK depends on a thorough eye assessment by your surgeon. However, for many individuals, PRK provides a safer, more comfortable option than LASIK, especially when preserving tear film stability and reducing the risk of chronic dryness is a priority.
Dry Eye Tests Your Surgeon Will Perform Before PRK
To make sure PRK is safe for you, your ophthalmologist will run several diagnostic tests.
Schirmer’s Test – Measures tear production.
TBUT (Tear Break-Up Time) – Checks how quickly tears evaporate.
Osmolarity Test – Evaluates tear-film stability.
InflammaDry Test – Checks for inflammatory markers (MMP-9).
Meibomian Gland Dysfunction (MGD) Assessment – Identifies blockages in oil glands.
Corneal Topography – Ensures your cornea is healthy and regular.
These tests help create a plan that supports your eyes both before and after surgery.
Preparing Your Eyes Before PRK
If you have dry eyes, preparing your eyes before PRK is an important step to ensure the best possible outcome. Your surgeon may recommend a pre-treatment plan aimed at optimising tear film stability and overall eye health before the procedure.
This plan can include using lubricating eye drops regularly, taking omega-3 supplements, and applying warm compresses to support natural oil production. Advanced therapies like Meibomian gland treatment (LipiFlow or IPL) or anti-inflammatory drops may also be suggested to reduce irritation and improve tear quality.
In some cases, punctal plugs can be used to help retain moisture, and maintaining a consistent eyelid hygiene routine can further stabilise the tear film. By addressing dryness beforehand, pre-conditioning your eyes helps ensure a smoother recovery and enhances the long-term comfort and effectiveness of PRK.
PRK Recovery for Dry Eyes: What to Expect
PRK recovery is slower than LASIK, but many people appreciate the stability it brings long-term.
Stage 1: First 3–5 Days
During the first few days after surgery, it’s normal to experience discomfort, blurry vision, and light sensitivity. Your eye will usually have a bandage lens in place to protect it and aid healing. Dryness is common at this stage, but using artificial tears regularly can help relieve irritation and support comfort.
Stage 2: Weeks 2–4
During weeks two to four, the surface of your eye continues to smooth, and your vision may fluctuate as healing progresses. Dryness gradually improves, though using eye drops is still recommended to maintain comfort and support the recovery process.
Stage 3: Months 2–6
Between two and six months after surgery, visual clarity from the laser treatment becomes more stable, and dryness reduces significantly as the corneal nerves regenerate naturally. By this stage, most patients report that their eyes feel the same as before surgery—or even better.
Managing Dryness After PRK
Your surgeon will give you a personalised aftercare plan, but common strategies include:
Preservative-free artificial tears – Use frequently during the first few months.
Punctal plugs – These tiny inserts reduce tear drainage and help retain moisture.
Warm compresses – Support oil production to prevent tear evaporation.
Omega-3 supplements –Help improve the quality of your tear film.
Humidifier use – Especially helpful during winter or prolonged screen time.
Avoiding air-conditioning and wind exposure – To prevent rapid tear evaporation.
Limiting screen time initially – Screens reduce blink rate and worsen dryness.
Can PRK Solve Dry Eyes?
While PRK doesn’t cure dry eyes, it is often a safer choice for people who already experience dryness. Unlike LASIK, PRK doesn’t involve creating a flap, which means there’s less disruption to corneal nerves that play a role in tear production. As a result, many patients notice more stable vision, fewer symptoms compared with contact lens use, and a lower risk of irritation.
PRK also avoids the flap-related complications that can exacerbate dryness after LASIK. For those with mild to moderate dry eyes that are properly managed, PRK can provide long-term visual clarity and increased comfort. With the right post-operative care, many patients find their eyes feel healthier and more comfortable over time.
Special Considerations for Severe Dry Eyes
For patients with severe or persistent dry eyes, especially when linked to conditions like Sjögren’s syndrome, extra precautions are necessary before considering PRK. Surgeons may recommend treatments to improve the ocular surface, such as punctal occlusion, autologous serum eye drops, or advanced therapies for meibomian gland dysfunction. These interventions help stabilise the tear film and create a healthier environment for healing after surgery.
In many cases, PRK can still be performed once dryness is managed effectively. However, if the tear film remains unstable despite treatment, laser surgery may need to be postponed, as operating on a compromised ocular surface can increase the risk of complications and affect visual outcomes.
Careful evaluation and personalised management are key to ensuring both safety and the best possible long-term results for patients with severe dry eyes.
PRK vs LASIK for Dry Eyes: Comparison Chart
Flap creation: PRK does not involve creating a corneal flap, while LASIK requires a flap to be created. Because LASIK disrupts more corneal nerves during flap creation, it can increase the risk of dry eyes after surgery.
Dry eye impact: PRK generally has a lower impact on dry eyes, making it more suitable for people who already experience dryness. LASIK, on the other hand, has a higher tendency to worsen dryness, especially in the early healing period.
Recovery time: PRK has a slower recovery time because the surface layer of the cornea needs to regenerate. LASIK offers a much faster recovery, often with clearer vision within a day or two.
Corneal stability: PRK provides higher corneal stability in the long term since there is no flap. LASIK offers good stability too, but it is slightly lower due to the presence of the flap.
Suitability for thin corneas: PRK is an excellent option for people with thin corneas. LASIK may not be suitable in such cases because it requires more corneal tissue.
Suitability for contact lens intolerance: PRK is often recommended for those who cannot tolerate contact lenses. LASIK may be suitable in some cases but not always ideal for patients with severe intolerance.
Long-term dryness risk: PRK carries a lower long-term risk of dryness, whereas LASIK has a higher chance of dryness persisting, especially in patients who already have dry eyes before surgery.
FAQs:
- Is PRK really safer than LASIK for people with dry eyes?
Yes, PRK is generally considered safer because it does not involve creating a corneal flap. During LASIK, nerves responsible for tear production are cut, which can reduce tear reflex and make dryness worse. PRK only affects the surface layer of the cornea, meaning far fewer nerves are disrupted. As a result, people with pre-existing dry eyes usually experience a gentler healing process and a lower risk of long-term dryness compared to LASIK. - Will PRK make my dry eyes worse permanently?
Most people do not experience permanent worsening of dry eyes after PRK. It can cause temporary dryness during the healing period, especially in the first few weeks, but the symptoms typically improve steadily as the corneal surface regenerates. Because the deeper nerves remain untouched, the tear film often becomes more stable with time. Long-term dryness is uncommon, especially when proper aftercare and tear-film treatment are followed. - How long does dryness last after PRK?
Dryness usually peaks in the first week as the epithelium heals, and then gradually improves over the next several weeks. Most people notice significant relief between two to six weeks, and by three to six months, the majority report that their eyes feel either the same as before surgery or noticeably better. The timeline can vary depending on your tear quality, lifestyle, and how consistently you follow your aftercare plan. - Can PRK cure my dry eyes completely?
PRK is not designed to cure dry eye syndrome, but it can allow you to enjoy vision correction without worsening your symptoms. Some patients even feel more comfortable after surgery because they are no longer wearing contact lenses, which often aggravate dryness. The main goal of PRK is to avoid additional nerve damage, making it a safer choice for people who already struggle with dryness. - If I have severe dry eyes, can I still get PRK?
Severe dry eyes require a careful evaluation before surgery. Many people with significant dryness can still have PRK once their tear film is stabilised with treatments like lubricating drops, punctal plugs, omega-3 supplements, or meibomian gland therapy. However, if the dryness is uncontrolled or linked to an autoimmune condition, your surgeon may recommend improving the ocular surface first or, in rare cases, avoiding laser surgery until the condition is better managed. - How does PRK affect the tear film during recovery?
Immediately after PRK, the tear film is slightly unstable because the surface layer of the cornea is healing. This can create fluctuations in clarity, a gritty sensation, or occasional burning. As the epithelium regenerates, the tears spread more evenly across the cornea and the stability gradually returns. Since the procedure does not cut the deeper nerves, the tear film typically recovers more naturally and completely compared with LASIK. - Can I use artificial tears after PRK if my eyes are already dry?
Absolutely, and in fact, it’s recommended. Preservative-free artificial tears are a key part of recovery because they help keep the surface moist and reduce discomfort. Using them regularly during the first few months keeps the tear film stable, speeds healing, and prevents irritation. Your doctor may also suggest additional therapies such as punctal plugs or warm compresses if dryness is more persistent. - Will screen time make dryness worse after PRK?
Yes, screen time can temporarily make dryness worse because it reduces your blink rate. After PRK, the eyes are more sensitive, and prolonged screen use may lead to faster tear evaporation. It’s best to take frequent breaks, follow the 20-20-20 rule, and use lubricating drops whenever your eyes feel strained. As healing progresses, most people find they can return to normal screen habits comfortably. - Is PRK painful for people with dry eyes?
The procedure itself is usually painless, but the first few days of recovery can feel more noticeable if you already have dryness. Some people describe it as a gritty, burning, or sandy sensation. These symptoms are managed with numbing drops, bandage contact lenses, lubricants, and medications provided by your surgeon. The discomfort generally improves significantly once the epithelium has healed. - How do I know if PRK is the right choice for my dry eyes?
The best way to determine suitability is through a detailed assessment that includes tear-film testing, corneal mapping, and an evaluation of your meibomian glands. If your dryness is mild to moderate and your corneal thickness is suitable, PRK is often the preferred option. If your dryness is more severe, pre-treatment may be needed to stabilise the ocular surface first. Your individual lifestyle, visual goals, and tear-film health all help determine whether PRK will give you safe, comfortable, long-term results.
Final Thoughts: Choosing the Safest Laser Option for Dry Eyes
Living with dry eyes can make the decision about laser vision correction feel overwhelming, but PRK often provides a safer and more comfortable pathway for long-term clarity. Because it avoids flap creation and disrupts fewer corneal nerves, PRK tends to offer more stability and less dryness for those already struggling with tear-film issues. With the right assessment, pre-treatment, and aftercare, many patients with mild to moderate dryness achieve excellent visual results without worsening their symptoms. If you’re considering PRK surgery in London and want to know if it’s the right option for your eyes, you’re welcome to reach out to us at Eye Clinic London to book a consultation.
References:
- Bower, K.S., Sia, R.K., Ryan, D.S., Mines, M.J. & Dartt, D.A. (2015) ‘Chronic dry eye in photorefractive keratectomy and laser in situ keratomileusis: manifestations, incidence, and predictive factors’, Journal of Cataract & Refractive Surgery, 41(12), pp. 2624–2634. https://pubmed.ncbi.nlm.nih.gov/26796443/
- Yahalomi, T., Spiegel, D., May, M., Nir-Cohen, G., Zadok, D., Levkovitch,-Verbin, H., Avni, I. & Varssano, D. (2023) ‘Dry eye disease following LASIK, PRK, and LASEK: an observational cross-sectional study’, Journal of Clinical Medicine, 12(11), 3761. https://www.mdpi.com/2077-0383/12/11/3761
- Zarei-Ghanavati, S., et al. (2025) ‘Dry eye after photorefractive keratectomy (PRK) and transepithelial photorefractive keratectomy: a comparative clinical study’, BMC Ophthalmology. https://pubmed.ncbi.nlm.nih.gov/40540100/
- Way, C. & Rüden, D.von (2024) ‘Transepithelial Photorefractive Keratectomy Review’, Vision, 8(1), 16. https://www.mdpi.com/2411-5150/8/1/16
- Bower, K.S., Sia, R.K., Ryan, D.S., Mines, M.J. & Dartt, D.A. (2015) ‘Chronic dry eye in PRK and LASIK: manifestations, incidence and predictive factors’, Journal of Cataract & Refractive Surgery, 41(12), pp. https://pmc.ncbi.nlm.nih.gov/articles/PMC5702539/

