Is Corneal Cross-Linking Right for You? What Keratoconus Patients Should Consider

Introduction: Understanding Keratoconus and the Role of Cross-Linking
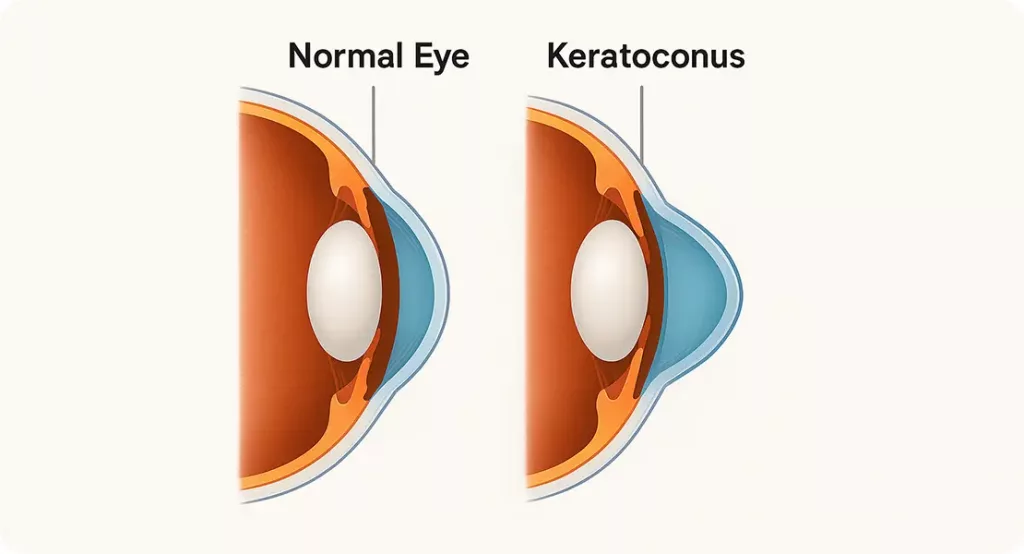
Keratoconus is a condition that causes the cornea — the clear front surface of the eye — to progressively thin and bulge outward into a cone-like shape. This irregularity leads to blurred, distorted vision, ghosting, light sensitivity, and increasing astigmatism.
In the UK, around 1 in 375 people are affected by keratoconus, though in some regions, like the Middle East and South Asia, the prevalence is significantly higher — as much as 1 in 84. It is also more common in patients of South Asian, Middle Eastern, and North African descent, and often runs in families.
Unfortunately, keratoconus is frequently misdiagnosed or diagnosed late. Patients may be prescribed new glasses repeatedly or even mislabelled as having “difficult astigmatism” for years before proper topography confirms the condition. As a result, many individuals reach moderate or advanced stages before treatment options are considered.
This delay can have serious consequences — once the cornea becomes too thin or distorted, treatment options become limited. Corneal cross-linking (CXL) offers a way to halt the condition and preserve vision if applied early. This article helps you understand whether cross-linking is right for you, by exploring its benefits, risks, timing, and recovery.
Why Cross-Linking Matters
Contact lenses and glasses help correct the symptoms of keratoconus, but they do not stop it from progressing. As the cornea thins, lenses may become difficult to fit, visual acuity may deteriorate, and some patients face the possibility of corneal transplantation.
Corneal Cross-linking is the only medical treatment currently available that can stop or slow down the progression of keratoconus. It works by strengthening the collagen fibres within the cornea, improving the structural integrity and resisting further bulging or deformation.
History of Corneal Cross-Linking
Corneal cross-linking was pioneered by Professor Theo Seiler and colleagues in Dresden, Germany in the late 1990s. The concept of strengthening biological tissue using light and photosensitisers emerged from orthopaedic and dermatological research. Prof. Theo Seiler, a German ophthalmologist and physicist, led the development of a technique to stiffen the cornea using ultraviolet A (UVA) light and riboflavin (vitamin B2). The first human corneal cross-linking (CXL) procedure was performed in 1998 at the Technical University of Dresden.
Seiler’s work built upon early research into riboflavin’s ability to absorb UVA and generate reactive oxygen species (ROS) that could induce new chemical bonds (cross-links) between collagen fibres. The goal was to halt the biomechanical weakening seen in keratoconus and similar corneal ectasias.
This became known as the Dresden Protocol, which remains the gold standard today:
- Epithelium-off treatment
- 30 minutes of riboflavin saturation
- 30 minutes of UVA exposure at 3 mW/cm²
Since then, clinical trials and long-term studies have validated cross-linking as the only effective intervention for slowing or halting keratoconus progression. The procedure has evolved with the introduction of accelerated, pulsed, and epithelium-on techniques, but the core principle remains unchanged.
Over the past 20 years, thousands of studies have confirmed its safety and efficacy.
How Cross-Linking Works: The Science Made Simple
The cornea owes its strength and shape to collagen fibres — long protein strands arranged in layers and held together by natural cross-links. In keratoconus, these fibres become weak or loosely connected, allowing the cornea to bulge and thin over time.
Corneal cross-linking introduces new covalent bonds between these collagen fibres, restoring structural integrity and reducing corneal elasticity.

Here’s what happens during the procedure:
- Topical anaesthetic drops are applied to numb the eye.
- Riboflavin (vitamin B2) is applied to the cornea for 30 minutes. It penetrates into the stromal layer, acting as a photosensitiser.
- The cornea is then exposed to UVA light (typically at 365 nm wavelength).
- UVA activates the riboflavin, generating reactive oxygen species. These ROS stimulate new cross-links between collagen molecules.
- As a result, the cornea becomes stiffer and more resistant to deformation — up to 3 to 4 times stronger biomechanically in lab studies.
- A bandage contact lens is placed on the eye for protection during healing.
- This is a day procedure, typically lasting around 60–90 minutes. You’ll be able to go home the same day.
This treatment essentially mimics and accelerates natural ageing, which is why keratoconus tends to stabilise later in life. Corneal Cross-Linking (CXL) provides a permanent “maturation” of the cornea’s collagen structure, locking it in place at an earlier, more stable phase.
Who Should Consider Cross-Linking?
Cross-linking is most effective for:
- Patients under 40 years old, though older patients may still benefit
- Individuals with early or moderate keratoconus
- Anyone with documented progression over 6–12 months
- Patients with corneal thickness over 400 microns (minimum safety threshold)
Cross-linking is not a vision correction procedure. It will not remove the need for glasses or lenses, but it is intended to preserve your current level of vision by halting further deterioration.
Why Timing Matters: The Case for Early Cross-Linking
In keratoconus, the window for intervention is critical. The earlier corneal cross-linking is performed — ideally during the early or moderate stages of the disease — the greater the likelihood of success in halting progression and preserving functional vision.
Here’s why timing is so important:
- Progression Can Be Rapid and Unpredictable
- Keratoconus doesn’t always progress slowly or steadily. In many patients — especially children and adolescents — the cornea can steepen significantly within a few months, leading to sudden changes in vision. Once the cornea becomes too thin or irregular, options like cross-linking may no longer be safe or effective.
- Early Cross-Linking Preserves Your Vision as it is Now
Cross-linking is not a vision correction procedure. It won’t reverse keratoconus, but it can help you keep the level of vision you currently have. If performed early, before the cornea becomes severely distorted or scarred, you are more likely to:- Keep wearing glasses or contact lenses comfortably
- Avoid needing custom or hard-to-fit lenses
- Prevent long-term dependence on surgical options
- The Cornea Responds Better in Early Disease
Studies show that corneal cross-linking is more effective when the corneal shape is less severely altered. If performed early:- The biomechanical stiffening effect is more uniform
- There’s less risk of scarring or haze
- Long-term visual outcomes are better
- Delays May Lead to Permanent Structural Changes
Once scarring develops or the cornea thins below the safe threshold (typically <400 microns), standard corneal cross-linking may not be possible. Modified “thin cornea protocols” exist, but they may be less effective and carry a higher risk of complications. - You May Avoid the Need for Future Transplant Surgery
Corneal grafting (DALK or PK) is reserved for advanced keratoconus, often when all other options fail. While these surgeries can restore vision, they involve:- Long recovery periods
- Risk of rejection or complications
- Lifetime follow-up
- Potential for suboptimal vision
Early corneal cross-linking drastically reduces the lifetime risk of requiring a transplant.
Don’t Wait for Vision Loss
If your scans show early signs of keratoconus, and particularly if those scans indicate progression, timely cross-linking could preserve your sight for life. Many patients regret not acting sooner, especially when vision becomes more difficult to correct with lenses.
Ask your specialist:
- Is my keratoconus progressing?
- Is my cornea still suitable for cross-linking?
- What’s the risk if I wait six more months?
Choosing early treatment often means choosing stability — and protecting not just your cornea, but your independence and quality of life.
Recovery and Healing
Day 1-3
The first 72 hours after epithelium-off corneal cross-linking are often the most challenging. Once the anaesthetic drops wear off, patients commonly experience moderate to severe discomfort, which can include:
- A strong foreign body sensation (as if sand or grit is in the eye)
- Stinging or burning
- Watery eyes or tearing
- Light sensitivity
- Difficulty opening the eye
- Blurry vision or reduced visual function
This discomfort occurs because the outer layer of the cornea (the epithelium) is deliberately removed during the procedure to allow riboflavin to penetrate. Until the epithelium regenerates — typically over 48 to 72 hours — the cornea remains exposed and sensitive.
Pain can be described as sharp or throbbing, particularly during the first 1–2 days. It may impact sleep and normal function. A bandage contact lens is placed over the eye during surgery to protect the cornea and promote healing, but it does not fully eliminate the sensation.
Management during this phase includes:
- Prescribed antibiotic and anti-inflammatory eye drops
- Oral pain relief (such as paracetamol or ibuprofen)
- Cool compresses to reduce discomfort
- Avoiding light exposure — wearing sunglasses, even indoors, may help
- Rest and reduced screen time
Patients are advised to rest in a dark room and avoid any rubbing or touching of the eye. The bandage lens is usually removed at the follow-up appointment once epithelial healing is complete, typically in a week time.
Days 4–7:
- Discomfort improves
- Bandage lens is removed by your clinician
- Vision remains variable
Week 2–4:
- Gradual visual recovery
- Most patients return to work/school during this period
- Regular use of antibiotic and anti-inflammatory drops continues
Month 1–3:
- Vision continues to stabilise
- Contact lenses may be refitted if needed
- Early signs of corneal flattening may begin to appear
- One month follow up appointment is usually arranged to monitor the healing process
Long term:
- Annual follow-up topographies are advised
- In most cases, no further intervention is needed
Patients with bilateral keratoconus often benefit from having both eyes treated at the same time, particularly when using newer accelerated protocols and with modern post-operative care. This minimises overall disruption and ensures consistent stabilisation.
Expanded Benefits of Cross-Linking
While the primary aim is to halt disease progression, cross-linking offers several additional benefits:
- Reduces the risk of needing a corneal transplant: Studies show that CXL decreases the lifetime likelihood of requiring a graft by 80–90%.
- Preserves current visual acuity: By stopping progression, CXL maintains the vision you have today.
- Improves lens fitting: Some patients experience improved lens stability and tolerance post-CXL, making scleral and RGP lenses easier to wear.
- Possible flattening effect: In 40–50% of cases, corneal steepening (Kmax) may reduce slightly, leading to modest improvements in visual acuity or refractive error.
- Long-term stability: Most patients treated early remain stable for 10+ years after a single treatment.
It’s important to note that cross-linking is not a refractive procedure. It does not eliminate the need for glasses or lenses, but it helps maintain your ability to use those tools effectively over time.
Expected Outcomes
The primary goal of cross-linking is to stop progression, not to improve vision. However, many patients do experience some visual benefit.
Success rates:
- Around 90% of patients show stabilisation after one procedure
- 45–50% may show mild flattening or visual improvement
- Fewer than 10% require retreatment within 5–10 years
The effect of CXL is considered long-lasting or permanent, especially if progression is caught early.
Risks and Considerations
Although cross-linking is considered safe and minimally invasive, it does carry potential risks:

- Delayed epithelial healing
- Corneal haze or scarring
- Infection (rare)
- Sterile inflammation
- Mild vision reduction (uncommon, usually temporary)
Patients with very thin corneas may require customised or “epithelium-on” protocols, which may be less effective. Your specialist will assess your corneal thickness and topography to determine eligibility.
Variations in Cross-Linking Techniques
While the Dresden Protocol (epithelium-off, 30-minute UV) is still the standard, other approaches are emerging:
- Accelerated cross-linking: stronger UV light for shorter duration
- Transepithelial (epi-on) corneal cross-linking: keeps the epithelium intact for quicker recover
Each has its pros and cons — but standard epithelium-off cross-linking remains the most evidence-based technique, especially for progressive disease.
Long-Term Care After Cross-Linking
- You’ll still need contact lenses or glasses
- Annual topography is recommended to monitor stability
- Avoid eye rubbing — it remains a risk factor
- Maintain dry eye treatment if necessary
- If keratoconus progresses after CXL (rare), retreatment may be discussed
Frequently Asked Questions
Is cross-linking painful?
The procedure itself isn’t painful due to numbing drops.
First 48 to 72 hours after Corneal cross-linking — particularly the epithelium-off version — can be painful. This is because the epithelium (the outer layer of the cornea) is removed during the procedure, leaving the underlying nerve endings temporarily exposed until the surface regenerates, which typically takes about 2 to 3 days.
The discomfort tends to peak within the first 24–48 hours, but in some individuals, it may last slightly longer — particularly if healing is slower. This phase is manageable with prescribed painkillers, anti-inflammatory drops, cool compresses, and a bandage contact lens placed over the eye for protection.
While the first few days can be challenging, most patients report that the pain is temporary and worth the long-term benefits, especially knowing the procedure can preserve their vision and potentially prevent more invasive surgery later in life.
Can I have both eyes treated at once?
Yes. Many clinics, including Eye Clinic London, routinely perform simultaneous bilateral cross-linking — treating both eyes during the same visit. This approach is increasingly popular for patients with bilateral keratoconus and simplifies logistics, especially for children, students, and those travelling from afar.
Whether simultaneous treatment is appropriate depends on:
- Corneal thickness in both eyes
- The stage of disease
- The patient’s overall health and tolerance
- The clinic’s protocol and your surgeon’s assessment
There’s no increased risk with bilateral treatment if performed correctly. Patients should expect similar recovery timelines for both eyes and may need additional support for a few days after surgery, particularly if both eyes are blurred initially.
How soon will I see results?
Cross-linking begins working at a cellular level immediately after the procedure, but visible outcomes take time.
If referring to vision, most patients experience blurred or reduced visual clarity for several weeks, especially during the epithelial healing phase. Any visual improvement, such as reduced steepening or better lens fit, typically becomes noticeable between 3 to 6 months, though this varies from person to person — and not all patients see a visual improvement.
If referring to disease stabilisation, this is assessed through follow-up scans taken at 3, 6, and 12 months. These scans monitor the cornea’s shape to confirm that the keratoconus has stopped progressing.
Is the result permanent?
Yes, in most cases. The cross-linked collagen is more stable, and retreatment is rarely needed. However, lifelong monitoring is still advised.
Can I wear contact lenses after cross-linking?
Most patients can safely resume contact lens wear around 3 to 4 weeks after the procedure — but this varies depending on how quickly the corneal surface heals and how stable the vision is.
Your ophthalmologist will assess the epithelial integrity and corneal surface at your follow-up appointments. Wearing lenses too early can interfere with healing, increase discomfort, or lead to complications such as corneal staining or infection.
Never restart lens wear on your own — your specialist will guide you and confirm when it’s clinically appropriate and safe to do so.
Are there people who should not have cross-linking?
Yes. Patients with:
- Corneas thinner than 400 microns
- Significant scarring
- Active eye infections
- Severe dry eye or autoimmune conditions
…may not be suitable candidates, or may require modified protocols.
What’s the alternative if I can’t have cross-linking?
Other treatments include:
- Intracorneal rings (INTACS)
- KeraNatural inlays
- Scleral lenses
- Corneal transplant (in advanced cases)
Does it stop the need for a transplant?
In most cases, yes. Cross-linking reduces the lifetime risk of needing a corneal graft by halting progression before the cornea becomes too distorted or scarred.
Will it improve my vision?
Corneal cross-linking is not designed to improve vision directly — its primary goal is to halt the progression of keratoconus, not reverse it.

However, some patients may experience a mild improvement in vision over time, typically within 3 to 12 months after the procedure. This improvement is usually the result of:
- Slight corneal flattening (reduction in steepness)
- Improved corneal symmetry
- Better tolerance or fit of contact lenses
However, this benefit is not guaranteed. The degree of improvement depends on the stage of the disease at the time of treatment, your corneal biomechanics, and how your eye responds to healing. Even without visual improvement, stabilising your condition means you are more likely to maintain your current vision long term, avoiding the need for more invasive procedures like corneal transplant.
Can I fly or travel soon after the procedure?
Yes. After the first 1–2 weeks of healing, you can fly. Be cautious about dry air and take your medication and drops with you.
Final Thoughts
Corneal cross-linking is a pivotal treatment in the management of keratoconus. It doesn’t restore vision — but it preserves it. When offered at the right time and under the right conditions, it can prevent decades of visual decline, difficult lens fittings, and in many cases, the need for a corneal transplant. If you’ve recently been diagnosed with keratoconus or have been told your scans are changing, speak to a corneal specialist. Ask about progression. Ask about timing. Ask about corneal cross-linking. Because when it comes to preserving vision, sooner is always better than later.
If you’re concerned about keratoconus or would like to learn more about corneal cross-linking, feel free to contact us at Eye Clinic London to book a consultation with one of our expert ophthalmologists.
References
- Wollensak, G., Spoerl, E. and Seiler, T., 2003. Riboflavin/ultraviolet‐A–induced collagen crosslinking for the treatment of keratoconus. American Journal of Ophthalmology, 135(5), pp.620-627. https://doi.org/10.1016/S0002-9394(02)02220-1
- O’Brart, D.P.S., 2017. Corneal collagen cross-linking: A review. Journal of Optometry, 10(2), pp.63–68. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5405582/
- Sykakis, E., Karim, R., Evans, J.R., Bunce, C., Amissah-Arthur, K.N., Patwary, S. and Allan, B.D., 2015. Corneal collagen cross-linking for treating keratoconus: a systematic review. Cochrane Database of Systematic Reviews, (3). Available at: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010621.pub2/full
- Raiskup, F., Theuring, A., Pillunat, L.E. and Spoerl, E., 2015. Corneal collagen crosslinking with riboflavin and ultraviolet-A light in progressive keratoconus: ten-year results. Journal of Cataract & Refractive Surgery, 41(1), pp.41–46. Available at: https://www.sciencedirect.com/science/article/abs/pii/S0886335014010612
- National Institute for Health and Care Excellence (NICE), 2013. Photochemical corneal collagen cross-linkage using riboflavin and ultraviolet A for keratoconus and keratectasia. Interventional procedures guidance [IPG466]. Available at: https://www.nice.org.uk/guidance/ipg466

